Asthma is a chronic disease that affects the airways that carry oxygen in and out of the lungs, making it hard to breathe.
People with asthma have inflamed airways which can result in symptoms such as shortness of breath, coughing, chest tightness, and wheezing. The severity of those symptoms can range from mild to life-threatening. There is no cure for asthma but, with proper management, most people can control their condition so that symptoms occur infrequently and have a minimal impact on their daily life.
In California:
- More than five million Californians have been diagnosed with asthma at some point in their lives.
- Almost 3 million currently have Asthma.
- Asthma rates increased dramatically during the last three decades.
- Every year more than 40,000 Californians are hospitalized because of asthma and African Americans are at greater risk for hospitalization and death compared to other racial groups.
- Hospitalization rates among children are much higher than other age groups.
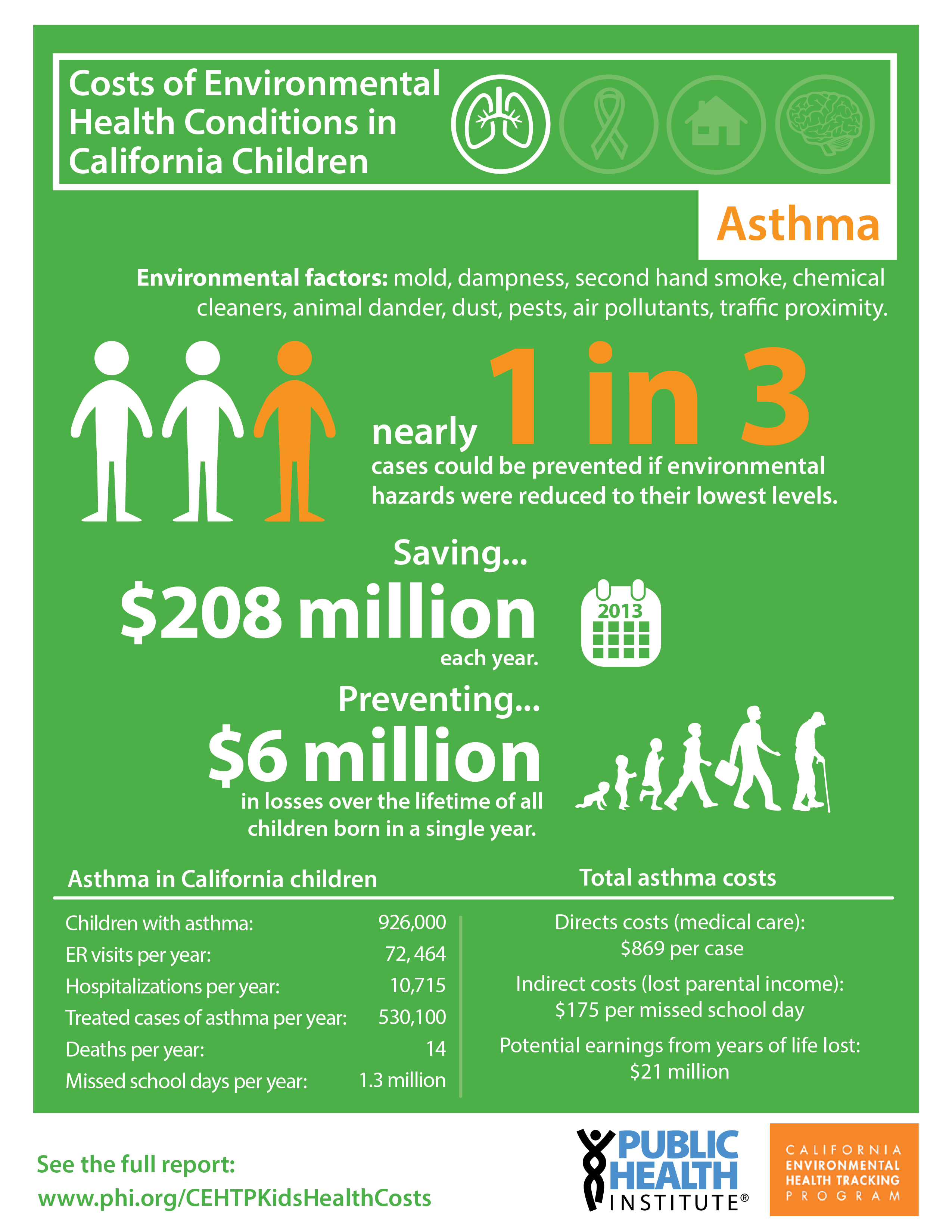
Although the exact causes of asthma are not fully understood, it is well-established that exposure to both outdoor and indoor environmental factors can trigger asthma attacks. Outdoor pollutants like traffic emissions, particulate matter, ozone, and diesel exhaust, along with indoor triggers such as mold and dust, are known contributors to asthma episodes.
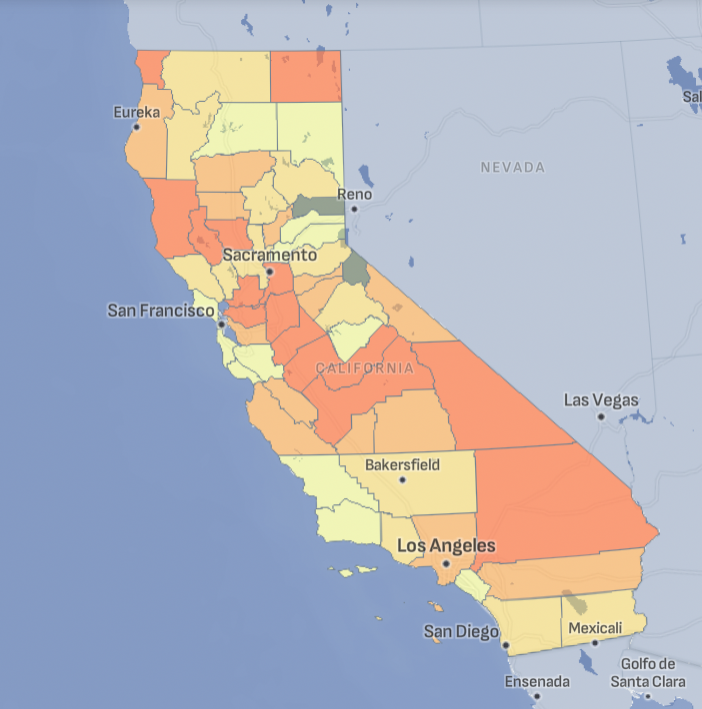
Asthma Across California
Tracking California provides a range of datasets on asthma, including emergency department visits and hospitalization rates, for counties across the state.
Asthma and the Environment
There is increasing evidence and awareness about the relationship between asthma and the environment. Since many non-environmental factors contribute to asthma, there have been efforts to estimate what proportion of the asthma burden is related to the environment. In a study conducted by the World Health Organization, it is estimated that 44% of the asthma burden worldwide is due to the environment. While there is some evidence that environmental factors can cause asthma, we know much more about indoor and outdoor environmental factors that can exacerbate asthma symptoms or trigger asthma attacks. Indoor air quality in the home and workplace is a concern for people with asthma.
Air Pollution
Air pollutants, including particulate matter, ozone, nitrogen dioxide, and diesel exhaust, can trigger symptoms among asthmatics. Children living in areas with higher traffic-related pollution in California have been shown to suffer significantly increased rates of asthma. Particulate matter from diesel engines has been shown to exacerbate asthma symptoms in children with asthma.
Pesticides
Exposure to certain pesticides can also trigger wheezing, coughing, and chest tightness and increase the risk of asthma morbidity in children with asthma.
Housing Conditions
Inadequate housing plays a significant role in exacerbating asthma, particularly as poor living conditions often expose residents to asthma triggers such as mold, dust mites, and pests. Additionally, older buildings with insufficient ventilation can concentrate indoor pollutants and allergens, further increasing the risk and severity of asthma attacks in occupants.
Climate Change
The increased frequency and severity of climate-related events, such as wildfires and dust storms, can create prolonged periods of poor air quality
In the U.S., an expert panel estimated that 30% of asthma exacerbations among children were related to the environment, costing the country $2.0 billion on an annual basis. Likewise in California, we estimated that 30% (20-41%) of asthma was attributable to the environment, with associated costs of $200 million per year.
Who is Vulnerable to Asthma?
Asthma impacts the population in many ways. Since many people can manage their symptoms or no longer experience symptoms, the number of people who have been diagnosed with asthma is different from the number of people who currently experience severe symptoms.
To understand the complete asthma burden in California, it's important to look at how many people have been diagnosed with asthma (lifetime asthma prevalence), how many are currently experiencing asthma attacks (current asthma prevalence), how people are using the healthcare system to manage their asthma, and the economic costs associated with asthma.
Different segments of the population bear a disproportionate burden of asthma. These disparities are significant by race and ethnicity, income, gender, age, and geographic location:
- American Indian/Alaska Native (AI/AN) adults have the highest asthma prevalence of any racial/ethnic groups, 40% higher than among whites.
- Compared to Whites, asthma hospitalization and ED visit rates are about four times higher for Blacks and asthma death rates are two times higher for Blacks.
- Asthma prevalence among American Indians/Alaskan Natives is more than 40% higher than among Whites
- Asthma prevalence among Blacks is about 30% higher than among Whites.
The reasons for these disparities are not fully understood. They may be related to living conditions, country of birth, access to healthcare, proximity to industrial areas or polluted sites, and occupational hazards that differentially affect various communities.
Asthma Related Projects
Asthma Publications
Associations between Ozone and Fine Particulate Matter and Respiratory Illness Found to Vary between Children and Adults. Implications for US Air Quality Policy [2019] Paul English, John Balmes
Use of health information in air pollution health research: past successes and emerging needs [2009] Thurston GD, Bekkedal MY, Roberts EM, Ito K, Pope CA, Glenn BS, Ozkaynak H, Utell
Are frequent asthma symptoms among low-income individuals related to heavy traffic near homes, vulnerabilities, or both? [2008] Ying-Ying Meng, Michelle Wilhelm, Rudolph P Rull, Paul English, Sheila Nathan, Beate Ritz
Environmental Public Health Tracking of Childhood Asthma Using California Health Interview Survey, Traffic and Outdoor Air Pollution Data [2008] Michelle Wilhelm, Ying-Ying Meng, Rudolph P Rull, Paul English, John Balmes, Beate Ritz
Traffic and outdoor air pollution levels near residences and poorly controlled asthma in adults [2007] Ying-Ying Meng, Michelle Wilhelm, Rudolph P Rull, Paul English, Beate Ritz