Maternal and infant health refers to the health and well-being of mothers and their newborns during pregnancy, childbirth, and the postnatal period.
In an ideal society, all babies should be born after a full-term pregnancy that is safe for both the pregnant parent and infant, and they should be positioned to thrive as their new lives begin.
Not all pregnancies continue to full-term, resulting in miscarriage, stillbirth, perinatal mortality or pre-term birth outcomes. Low birthweights as well as infant mortality (neonatal and post neonatal) are also poor outcomes included within infant health.
These health outcomes are some of the most widely watched indicators of the public's health. Many of these outcomes are profoundly affected by the social and physical environments in which pregnant people and children live, and can be affected by access to skilled healthcare providers, chronic health conditions, as well as inadequate prenatal care and nutritional deficiencies during pregnancy.
Efforts to improve maternal and infant health focus on providing comprehensive prenatal and postnatal care, ensuring access to skilled healthcare, promoting proper nutrition, and addressing social determinants of health.
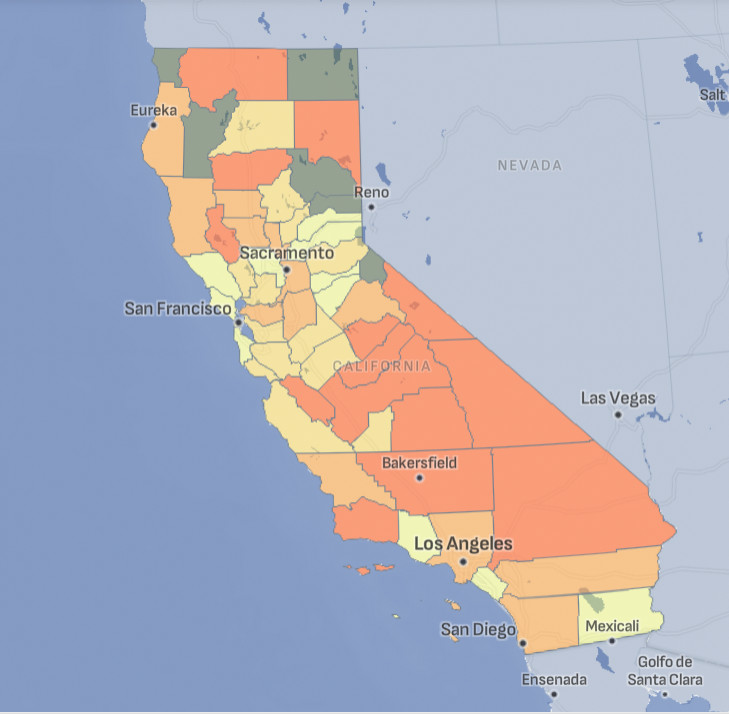
Maternal and Infant Health Across California
Tracking California provides datasets on ten indicators related to maternal and infant health, including pre-term births and low birthweights, for counties across the state.
Understanding Maternal and Infant Health Outcomes and Indicators
Key outcomes and indicators of poor maternal and infant health include:
Maternal health
This includes the health of women during pregnancy, childbirth, and the postpartum period. Key factors include access to prenatal care, management of pregnancy-related conditions, safe delivery practices, and postpartum care to ensure the mother's physical and mental health.
Key indicators used to study maternal health include:
Interruption of pregnancy, which may occur spontaneously or be medically induced when the health of the pregnant person or their baby is threatened:
- Preterm birth is a singleton birth prior to 37 weeks of gestation (about 8.5 months).
- Very preterm birth is a singleton birth prior to 32 weeks of gestation.
Reduced growth of the fetus during pregnancy:
- Full-term low birthweight birth is a singleton birth born at full term (37 weeks of gestation) and with a birthweight less than 2,500 grams.
- Very low birthweight birth is a singleton birth born with a birthweight of less than 1,500 grams.
Infant health
This focuses on the health of newborns and infants, typically up to one year of age. It includes ensuring proper nutrition, immunizations, regular health check-ups, and addressing any congenital conditions or illnesses to promote healthy development.
Key indicators used to study infant health include:
- Mortality rates:
- Infant mortality, which is a death of an infant less than one year of age.
- Neonatal mortality, which is a death of an infant less than 28 days of age.
- Postneonatal mortality, which is a death of an infant between 28 days and 12 months of age.
- Perinatal mortality, which includes both stillbirths after 28 completed weeks of pregnancy and live births prior to 7 days of age.
To address poor outcomes in maternal and infant health outcomes, preventive measures and interventions are crucial for both maternal and infant health and include education on proper nutrition, breastfeeding, family planning, and the prevention and treatment of diseases and infections.
The overall goal of maternal and infant health initiatives is to reduce maternal and infant mortality rates, prevent health complications, and promote the long-term health and well-being of both mothers and their children.
Public Health researchers use data from both birth records and death records to keep track of the health of communities. Outcomes not directly related to health but that may reflect conditions in a community, such as fertility rates and sex ratios at birth are also collected.
Maternal and Infant Health and the Environment
The socio-economic determinants of poor maternal and infant heath outcomes are widely studied in epidemiological research, however there are comparatively fewer studies that understand the links between these outcomes and the environment.
Poor maternal and infant health outcome indicators can used able to explore what potential environmental factors impact maternal and infant heath, learning from previous research to identify potential harmful causes. For example, it has long been known that children born to people exposed to tobacco smoke during pregnancy are at higher risk for both prematurity and reduced fetal growth. Furthermore, workplace exposures (for both parents) to hazardous substances such as lead or welding fumes are also associated with adverse outcomes.
Studies have focused on prominent environmental factors, including:
Air pollution: Exposure to pollutants such as particulate matter, nitrogen dioxide, and sulfur dioxide can increase the risk of respiratory issues, preterm birth, and low birth weight in infants, as well as complications during pregnancy for mothers.
- This can include traffic as a key source of ambient air pollution exposure.
Water quality: Contaminated water sources can lead to waterborne diseases, which can cause dehydration and malnutrition in both mothers and infants, and increase the risk of birth defects, low birthweights and pregnancy complications.
Chemical exposure: Exposure to harmful chemicals, including pesticides such as diazinon and propoxur, chlorpyrifos, and DDT, heavy metals (like lead and mercury), and industrial products, can adversely affect fetal development and maternal health, increasing the risk of birth defects, stillbirths, and other complications.
- This can include living near a hazardous waste landfill.
Whilst traditionally, studies have focused on small-scale data collection (i.e., collecting samples from the pregnant person or from their surroundings and examine them for evidence of exposure), large-scale studies are becoming more prominent in research with exposures to environmental factors inferred based on where people live during their pregnancy from birth records.
These large-scale data analysis enables the study of maternal and infant health outcomes over longer time periods and greater spatial scales but are unable to capture fine-scale movements of individuals and their exposure to harmful environmental factors. Large-scale studies however may begin to provide a greater understanding on how a multitude of factors may contribute collectively to poor maternal and infant health outcomes; currently, most studies will focus on a single factor, even though most pollutants nearly aways occur in combinations.
Definitive research on the links between the environment to poor maternal and infant health outcomes is still in progress.
Who is Vulnerable to Poor Maternal and Infant Health Outcomes?
In the U.S., several groups are particularly vulnerable to poor maternal and infant health outcomes:
- Low-income individuals Economic challenges can limit access to quality healthcare, nutritious food, and safe living conditions, all of which are crucial for healthy pregnancies and infant development.
- Racial and ethnic minorities African American, Native American, and Hispanic women often face higher rates of maternal and infant mortality and morbidity due to systemic healthcare disparities, socioeconomic factors, and discrimination.
- Teen mothers Adolescents are at higher risk for complications during pregnancy and childbirth, partly due to biological factors and partly due to limited access to prenatal care and education on healthy practices.
- Rural residents Women living in rural areas may have limited access to healthcare facilities and specialists, leading to inadequate prenatal and postnatal care and increased risk of complications.
- Uninsured or underinsured individuals: Lack of health insurance can prevent women from receiving necessary prenatal and postnatal care, increasing the likelihood of untreated health issues and poor outcomes for both mothers and infants.
- Women with pre-existing health conditions: Chronic conditions such as diabetes, hypertension, and obesity can complicate pregnancy and increase the risk of adverse outcomes for both mother and child.
- Immigrant populations: Language barriers, lack of familiarity with the healthcare system, and potential legal concerns can prevent immigrant women from accessing adequate maternal and infant healthcare services.
- Homeless individuals: Homelessness can lead to poor nutrition, exposure to environmental hazards, and lack of consistent healthcare, all of which can negatively impact maternal and infant health.
Efforts to improve maternal and infant health outcomes for these vulnerable groups include expanding access to healthcare, addressing social determinants of health, and implementing targeted public health interventions.
Maternal and Infant Health Related Projects
Maternal and Infant Health Publications
Is in utero exposure to maternal socioeconomic disadvantage related to offspring ovarian reserve in adulthood? [2018] Maria E. Bleil, Paul English, Jhaqueline Valle, Nancy F. Woods, Kyle D. Crowder, Steven E. Gregorich, Marcelle I. Cedars
Residential Agricultural Pesticide Exposures and Risks of Preeclampsia [2018] Shaw GM, Yang W, Roberts EM, Aghaeepour N, Mayo JA, Weber KA, Maric I, Carmichael SL, Winn VD, Stevenson DK, English PB.
Residential Agricultural Pesticide Exposures and Risks of Spontaneous Preterm Birth [2018] Gary Shaw, Wei Yang, Eric Roberts, Susan Kegley, David Stevenson, S Carmichael, Paul English
Hypospadias and residential proximity to pesticide applications [2013] Carmichael SL, Yang W, Roberts EM, Kegley SE, Wolff C, Guo L, Lammer EJ, English P, Shaw GM
Other Maternal and Infant Health Resources

CDPH Maternal, Child and Adolescent Health (MCAH) Division
The Maternal, Child and Adolescent Health (MCAH) Division works to improve the health and well-being of women, infants, children and adolescents throughout the state. Many programs and initiatives serve California's diverse populations and regions, providing resources, information and data for physical, emotional, mental and social health.

CDC Division of Reproductive Health
CDC's Division of Reproductive Health provides scientific leadership in the promotion of women's health and infant health before, during, and after pregnancy.

